See all > Business solutions
Solving the riddle: how telehealth can make Canada a leader in timely healthcare
Canadians report the longest wait times for healthcare, yet less than half of Canadian doctors work full-time according to Statistics Canada. The cure for becoming a leader in timely access to care may not be as simple as “adding more doctors”.
We believe the solution to improving access to care lies in our ability to innovate. We need to embrace emerging technologies and telehealth to make better use of the physicians that already serve our communities.
Telehealth (aka telemedicine, e-health) is the remote delivery of healthcare using interactive text, audio, and video technology. It has the power to transform our healthcare delivery models, and create space for quicker and more comfortable access to care. However, while telehealth has seen massive adoption in other countries, the adoption rate in Canada is less than 1%.
Understanding wait times in Canadian healthcare
Canadians are generally happy with the quality of care received once they see a doctor. However, we consistently rank below all other developed countries when it comes to wait times to see the doctor. This is according to CIHI, the Canadian Institute for Health Information, which evaluates the performance of our healthcare system.
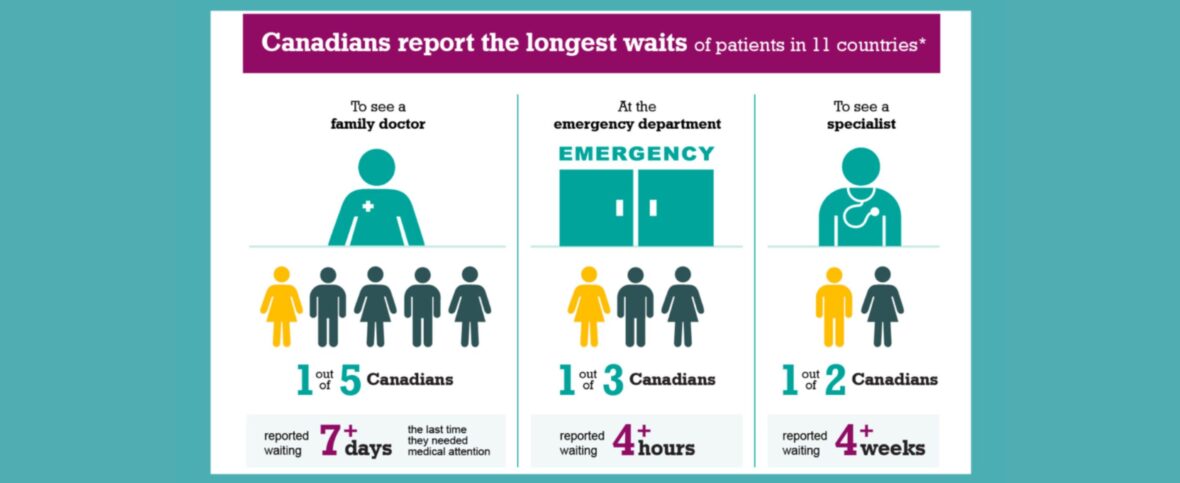
Key insights from the latest Canadian CIHI study:
- 20% reported waiting +7 days to see a family doctor the last time they needed medical attention
- 43% were able to receive same or next day access to care
- 33% reported waiting +4 hours at the ER
- 50% reported waiting +4 weeks to see a specialist
- 41% were not able to get a same day answer when they contact their regular doctor’s office with a medical concern
The lack of access during alternative times, such as after hours or during weekends, leaves patients with limited options. Instead of attending their family physicians, patients end up relying on walk-in clinics or the emergency room. 41% of Canadians say they use the emergency room for conditions their family physician could have treated, had they been available. This puts an unnecessary financial strain on our healthcare system, as patients with routine issues turn to other more costly means.
So why don’t more Canadian doctors work full-time?
The demand from our aging and growing population on the healthcare system results in limited funding for investment in healthcare resources. Doctors, especially specialists, rely on operating rooms, equipment, hospital beds, nurses, and other infrastructure to provide care. For example, 178 fully trained orthopaedic surgeons in Canada are unemployed; 78% of newly-graduated ENT specialists (ear, nose and throat) failed to find a job due to lack of funding. Yet the wait times for specialist care are +4 weeks for 50% of Canadians.
In primary care, doctors continue to see a reduction in billing rates and earnings which makes it difficult to cover the costs of operating clinics, especially during evening and weekend hours.
How can telehealth help?
The majority of common primary care issues can be treated solely with a visual or verbal examination. Technologies like Maple create space for doctors to see and treat patients right in their home, whether it’s by phone, videoconferencing, or other means of instant communication.
Doctors working under full capacity in the physical world can now provide extra care at no additional cost. This means they do not need to hire additional staff or incur costs to run a clinic overtime, one of the greatest obstacles to expanding after hours availability.
For patients, telehealth means quicker and more comfortable access to care. Telehealth empowers a cancer patient to speak to an oncologist about their diagnosis at any time. It allows a worried parent to get a physician’s advice from home at 2AM instead of making a potentially expensive and inconvenient trip to a local ER.
Telehealth is a budding industry in the health provision ecosystem. Discoveries and ventures have, and will continue to lead groundbreaking developments in healthcare. For example, “wearables” and innovation in remote monitoring devices that measure vital signs will even further increase the rate of remote diagnosis and treatment. This means up to 126 million visits to Canadian clinics or hospitals can be prevented and treated much quicker in the community.
By expanding physician capacity to provide care and creating better patient experiences, telehealth can significantly lead to better access to care.
Maple: Our mission is to help people feel better faster, while empowering patients with more healthcare choice and control.
Trusted by millions of Canadians
Get started now

We're trusted by millions of Canadians
Join millions of Canadian families who enjoy 24/7 access to medical care within minutes.
Get started now4.6 score
5K+ Trustpilot reviews
Do you need medical care today?
Trusted, experienced doctors and nurse practitioners are ready to see you.
